Demystifying the Credentialing Process: Your Essential Guide to Healthcare Provider Credentialing
Healthcare provider credentialing is a crucial aspect of the medical profession, ensuring that doctors, therapists, and other healthcare professionals meet specific standards and qualifications. BCBS credentialing process , also known as medical credentialing or provider credentialing, plays a significant role in ensuring quality care and patient safety.
In the complex world of healthcare insurance, insurance credentialing becomes equally important. Healthcare providers need to go through insurance credentialing to be eligible for reimbursement from insurance companies for the services they provide. This process involves evaluating and verifying a provider's qualifications, experience, and compliance with insurance guidelines.
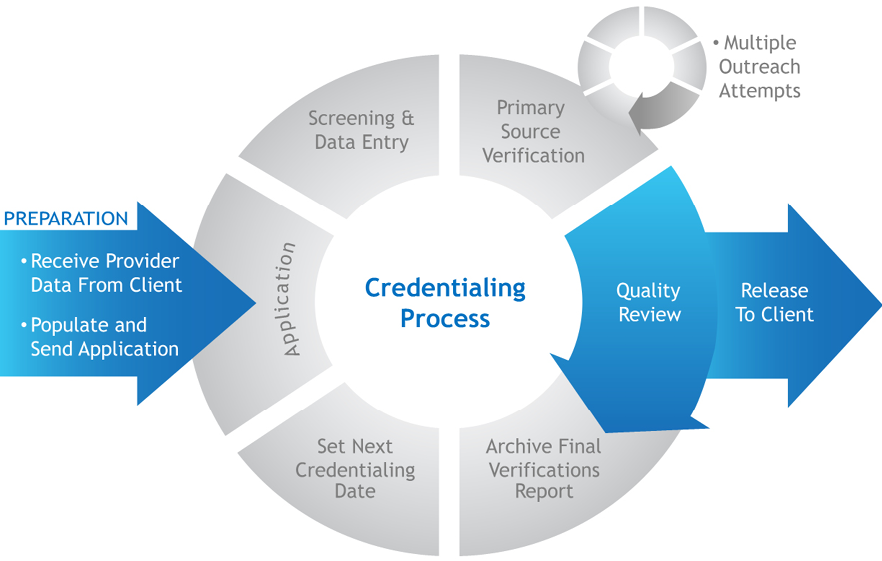
Understanding the credentialing process in healthcare is essential for both providers and insurance companies. It involves a series of steps that providers must navigate to become credentialed and participate in insurance networks. From gathering the necessary documents to completing applications and undergoing extensive reviews, the process can be time-consuming and daunting.
To ease this burden, many providers turn to insurance credentialing companies that specialize in guiding healthcare professionals through the intricacies of credentialing. These companies streamline the process, ensuring that all necessary information is gathered, applications are accurately completed, and deadlines are met.
In this article, we will demystify the credentialing process, providing you with a comprehensive guide to healthcare provider credentialing. We will explore the key aspects of medical credentialing, provider credentialing, and insurance credentialing, shedding light on the steps involved and offering insights into best practices. Whether you are a doctor seeking to navigate the credentialing process or an insurance company looking for effective credentialing solutions, this article is your essential resource.
Understanding the Credentialing Process
Credentials play a crucial role in the healthcare industry, ensuring that providers meet the necessary requirements to deliver quality care. Aetna credentialing specialist involves verifying and assessing the qualifications, experience, and competency of healthcare professionals. This ensures that healthcare providers, such as doctors, can offer their services and receive payment from insurance companies.
The first step in the credentialing process is gathering all the necessary information and documentation. Oscar health insurance complaints includes education and training certificates, licenses, malpractice insurance, and references. Once these documents are collected, they are carefully reviewed and verified to ensure accuracy and legitimacy.
Next, the credentialing process involves a thorough evaluation of a provider's qualifications. This evaluation may include checking for any past malpractice claims, disciplinary actions, or sanctions. Insurance companies rely on this evaluation to determine if a provider is eligible to join their network and if their services will be covered under their policies.
Finally, after the evaluation is complete, the provider's information is entered into a credentialing database, making it accessible to insurance companies and other relevant entities. This allows healthcare providers to become eligible for insurance reimbursement and participate in insurance panels for serving patients.
Understanding the credentialing process is essential for healthcare providers as it ensures that they meet the necessary standards and qualifications to practice medicine. It also allows insurance companies to make informed decisions about which providers to include in their networks. By completing this process, both healthcare providers and insurance companies can work together to provide quality care to patients.
Key Components of Healthcare Provider Credentialing
Credentialing is an essential process in the healthcare industry, ensuring that healthcare providers meet the necessary requirements to deliver quality care and be reimbursed by insurance companies. In this section, we will explore the key components of healthcare provider credentialing.
Verification of Education and Training: One of the crucial components of credentialing is verifying the education and training of healthcare providers. This involves confirming their medical degree, residency training, and any additional certifications or specializations they hold. By verifying their educational background, healthcare organizations can ensure that providers have the necessary knowledge and skills to deliver competent care.
License and Insurance Verification: To practice medicine, healthcare providers must hold an active and unrestricted license in the state where they practice. During the credentialing process, the provider's license is verified with the issuing authority to ensure compliance. Additionally, insurance companies require providers to carry malpractice insurance, and this coverage is also verified as part of the credentialing process.
Professional References and Work History: Another essential component of healthcare provider credentialing is gathering professional references and verifying the provider's work history. This helps assess the provider's clinical competence and professionalism. Providers may be asked to provide references from colleagues, supervisors, or previous employers who can provide insights into their clinical skills and interpersonal qualities.
Through these key components, healthcare provider credentialing aims to ensure that patients receive care from qualified and competent providers. By verifying education, licenses, insurance coverage, and work history, healthcare organizations can maintain high standards of patient safety and quality of care. Credentialing acts as a vital step in the healthcare system, promoting trust and integrity in the delivery of medical services.
Choosing the Right Credentialing Service
Finding the right credentialing service is crucial for healthcare providers and medical practices to ensure a smooth and efficient credentialing process. With a myriad of options available, it's essential to consider several factors before making a decision.
Firstly, it's important to look for a credentialing service that specializes in healthcare provider credentialing. This ensures that they have expertise and experience specifically in the field of medical credentialing, understanding the unique requirements and regulations involved. By choosing a service that focuses on healthcare credentialing, providers can have peace of mind knowing that their credentialing needs are in capable hands.
Secondly, consider the reputation and track record of the credentialing service. Look for companies that have a proven history of successful credentialing outcomes and positive reviews from satisfied clients. This can be an indicator of their reliability, professionalism, and ability to navigate through the complex credentialing process efficiently.
Lastly, it's important to consider the level of customer support and communication offered by the credentialing service. A responsive and supportive team can make a significant difference in ensuring a streamlined credentialing experience. Look for services that provide personalized assistance, prompt response times, and clear communication throughout the entire credentialing process.
By considering these factors and thoroughly researching different credentialing service providers, healthcare providers and medical practices can confidently choose a service that aligns with their specific needs and requirements. It's essential to select a service that is dedicated to efficiently managing and completing the credentialing process while providing exceptional support to healthcare professionals.